Eye Conditions
Diabetic Retinopathy (Non-Proliferative)
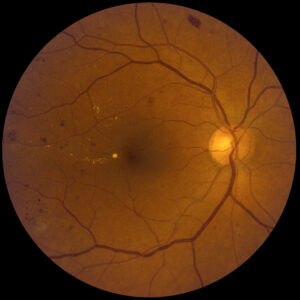 Diabetes can damage the blood vessels in the retina, the light-sensitive tissue that lines the back of the eye, weakening the vessel wall. These weak areas can balloon outward, called microaneurysms. Microaneurysms can leak tissue fluid into the surrounding retina, causing it to swell. They can also break and bleed, causing retinal hemorrhage. Fatty deposits, called lipoprotein can leak from microaneurysms as well, leading to yellowish deposits in the retina called exudates. Some blood vessels an also clot, or occlude and cause the surrounding retina to appear white. These areas are referred to as cotton-wool spots.
Diabetes can damage the blood vessels in the retina, the light-sensitive tissue that lines the back of the eye, weakening the vessel wall. These weak areas can balloon outward, called microaneurysms. Microaneurysms can leak tissue fluid into the surrounding retina, causing it to swell. They can also break and bleed, causing retinal hemorrhage. Fatty deposits, called lipoprotein can leak from microaneurysms as well, leading to yellowish deposits in the retina called exudates. Some blood vessels an also clot, or occlude and cause the surrounding retina to appear white. These areas are referred to as cotton-wool spots.
If any of the aforementioned conditions exist in or near the center retina, called the macula (responsible for detail vision) patients will experience blurred vision that is not correctible with glasses. Reports of “missing areas” in the vision are also common in patients with diabetic retinopathy and macular edema, or swelling in the macula.
Laser treatment or photocoagulation can be performed to cauterize these leaking vessels, and prevent them from causing more edema, and allow the body to absorb the existing fluid in the retina.
Diabetic Retinopathy (Proliferative)
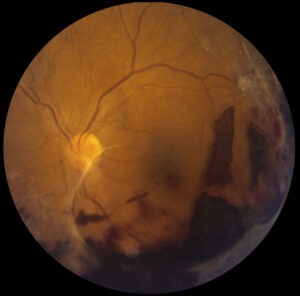 Sometimes large areas of the retina can begin to lose circulation as the small vessels or capillaries in the retina are damaged from diabetes. These areas of unhealthy retina are referred to as areas of nonperfusion. The body can respond to these areas and try to return blood flow by growing new, abnormal blood vessels on the surface if the retina. This is called proliferative retinopathy. The new, abnormal blood vessels grow quickly and can also leak and bleed, sometimes filling the eye with blood, called vitreous hemorrhage. The vessels can also grow into the vitreous (a clear, jelly-like substance that fills the inside of the eye) and create scar-like membranes that can contract and pull the retina out of place. Proliferative retinopathy is a very serious complication of diabetes, as it can lead to total loss of vision or even loss of the eye itself if not caught in its early stages.
Sometimes large areas of the retina can begin to lose circulation as the small vessels or capillaries in the retina are damaged from diabetes. These areas of unhealthy retina are referred to as areas of nonperfusion. The body can respond to these areas and try to return blood flow by growing new, abnormal blood vessels on the surface if the retina. This is called proliferative retinopathy. The new, abnormal blood vessels grow quickly and can also leak and bleed, sometimes filling the eye with blood, called vitreous hemorrhage. The vessels can also grow into the vitreous (a clear, jelly-like substance that fills the inside of the eye) and create scar-like membranes that can contract and pull the retina out of place. Proliferative retinopathy is a very serious complication of diabetes, as it can lead to total loss of vision or even loss of the eye itself if not caught in its early stages.
Proliferative diabetic retinopathy, in early or moderate stages can be treated with laser, or photocoagulation. Rather than direct treatment of vessels as can be done with non-proliferative retinopathy, patients with proliferative disease are treated first with panretinal photocoagulation. This type of laser involves creating hundreds of tiny burns in the outer or peripheral retina. This indirectly causes the new abnormal vessels to regress, or shrink, reducing the chances of vitreous hemorrhage.
Severe cases of proliferative retinopathy can not be treated with laser alone. If vitreous hemorrhage already exists, the surgeon cannot see details of the back of the eye due to the murky view from blood mixed with the vitreous. In this case, an outpatient surgery called a vitrectomy can be performed in order to remove the blood and release any vitreous membranes. The vitreous gel is also removed, and the eye is filled with a clear saline solution. The surgeon can then do the needed laser treatment in the operating room.
Age-Related Macular Degeneration (Dry)
 Age-related macular degeneration (AMD or ARMD) is the leading cause of central vision loss in people over fifty-five years of age. The macula is the central part of the retina that is responsible for detail vision and reading. Aging changes can occur in the macula, resulting in thin, damaged areas of retina, similar to aging changes experienced on the skin. This is known as the “dry” type of AMD.
Age-related macular degeneration (AMD or ARMD) is the leading cause of central vision loss in people over fifty-five years of age. The macula is the central part of the retina that is responsible for detail vision and reading. Aging changes can occur in the macula, resulting in thin, damaged areas of retina, similar to aging changes experienced on the skin. This is known as the “dry” type of AMD.
Dry AMD is the most common type of macular degeneration, gradually causing very slow vision loss over many years. While there is no known treatment for the dry type of AMD, most physicians recommend patients maintain a healthy diet and do not smoke. Protecting the eyes from ultraviolet radiation in sunlight is generally thought of as helpful.
Age-Related Macular Degeneration (Wet)
 Sometimes the body can react to dry AMD by growing new, abnormal blood vessels into the retina from the layer below called the choroid. This is called choroidal neovascularization. These abnormal blood vessel networks can leak fluid and blood into and under the retina.
Sometimes the body can react to dry AMD by growing new, abnormal blood vessels into the retina from the layer below called the choroid. This is called choroidal neovascularization. These abnormal blood vessel networks can leak fluid and blood into and under the retina.
The presence of abnormal vessels is known as “wet” AMD. Wet AMD usually causes severe loss of central vision very quickly. Patients report sudden dark or gray, blurry or distorted areas in their central vision.
Until recently there was little successful treatment of wet AMD. Now wet AMD is treated with a special injectable medication that causes the new leaky blood vessels to “dry up” and regress. Most patients who undergo treatment stabilize or improve visually, many enjoying dramatic visual improvement.
Posterior Vitreous Detachment
The vitreous is a clear gel or jelly-like substance that fills the eye and gives it its shape. It has a consistency similar to egg white. In young people, the vitreous is very thick and gel-like. As an individual ages the vitreous begins to contract and liquefy, and may separate from the retinal surface. This can also be induced by trauma, such as being hit with a soccer or tennis ball.
When the separation occurs, the patient may notice flashes of light in the edges of the vision. These peripheral flashes are caused by pulling on the retina as the vitreous detaches. The patient also usually reports sudden onset of floaters in the vision, from dark, pepper-like specks to large, hair-like strands that float across the vision with movement. Although most require no treatment, posterior vitreous detachments (PVD) can be very serious and lead to retinal tears and detachment. This is why dilated retinal examination is important soon after onset of symptoms.
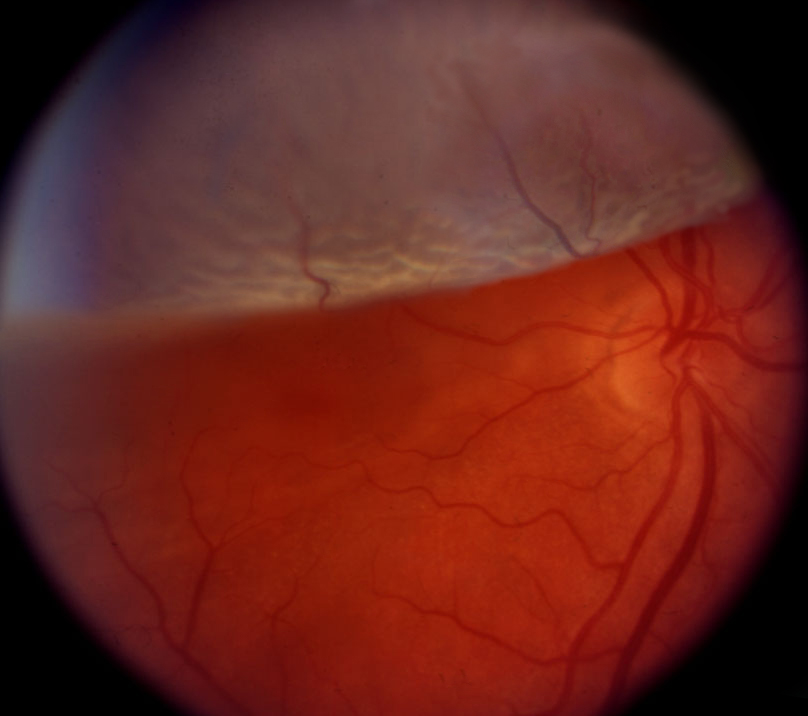
Retinal Tears and Holes
 The retina is the light-sensitive tissue that lines the inside wall of the eye. It is responsible for converting light and color to electrical signals that are interpreted by the brain as vision. In some cases, such as posterior vitreous detachment, the retina can tear as the vitreous tries to pull away (PVD). This torn retina can allow the fluid in the eye to seep through the tear and fill the space behind the retina, causing the retina to separate, known as retinal detachment.
The retina is the light-sensitive tissue that lines the inside wall of the eye. It is responsible for converting light and color to electrical signals that are interpreted by the brain as vision. In some cases, such as posterior vitreous detachment, the retina can tear as the vitreous tries to pull away (PVD). This torn retina can allow the fluid in the eye to seep through the tear and fill the space behind the retina, causing the retina to separate, known as retinal detachment.
Retinal holes are similar to tears and can form in areas of thin retina, usually in the peripheral, or side retina. Patients who are very nearsighted or myopic are at higher risk for developing retinal holes and tears because their peripheral retina is usually much thinner than that of the average person.
Patients who develop retinal tears usually report flashes of light and floaters in the vision.
Retinal tears and holes can be treated with laser if diagnosed early, usually in the doctor’s office. The tear or hole is surrounded by rows of small laser burns, thus “tack-welding” the retina in place and preventing retinal detachment.
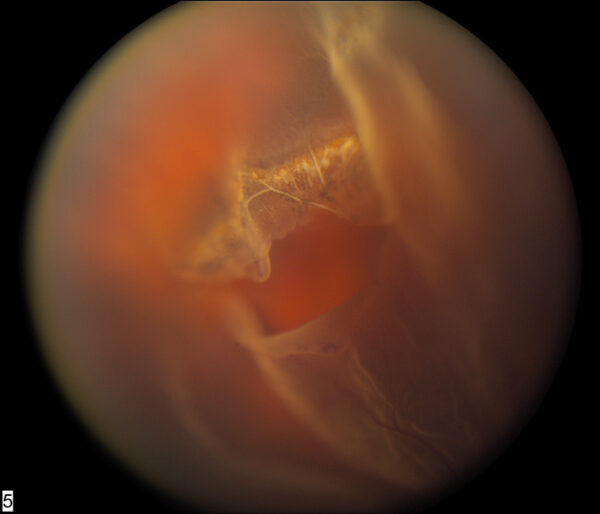
Retinal Detachment
 The retina is the light-sensitive tissue that lines the inside wall of the eye. It is responsible for converting light and color to electrical signals that are interpreted by the brain as vision. In some cases the retina can become separated from the wall of the eye, either from traumatic or natural causes (PVD, Retinal Tear).
The retina is the light-sensitive tissue that lines the inside wall of the eye. It is responsible for converting light and color to electrical signals that are interpreted by the brain as vision. In some cases the retina can become separated from the wall of the eye, either from traumatic or natural causes (PVD, Retinal Tear).
If this occurs, the patient usually notices a dark, veil-like shadow over a portion of the vision. The shadow can begin in any edge of the vision, and may slowly progress toward the center vision, or point of fixation. Some patients report a blurry, distorted area rather than a dark veil. Retinal detachment is a very serious, sight-threatening condition that must be diagnosed and treated quickly in order to preserve the patient’s vision. In most cases, if treated quickly patients can potentially regain all of their vision.
Repair of retinal detachment can vary from in-office laser treatment to outpatient surgery in the operating room.
Macular Pucker
 The macula, the center part of the retina is responsible for detail vision. In some cases a thin layer of cells can form a transparent membrane on the surface of the macula. It is not entirely understood why this membrane forms, though it is usually a gradual process.
The macula, the center part of the retina is responsible for detail vision. In some cases a thin layer of cells can form a transparent membrane on the surface of the macula. It is not entirely understood why this membrane forms, though it is usually a gradual process.
This membrane can contract, pulling the retinal surface with it, forming a wrinkled or “puckered” appearance. When light enters the eye and hits the wrinkled surface, the patient notices blurry and distorted vision. Straight lines may appear wavy; images such as faces may appear out of proportion. Severe cases may result in double vision.
Treatment consists of an outpatient procedure called a vitrectomy and membrane peel. The vitreous gel that fills the eye is removed and replaced with a special saline solution. The surgeon then carefully peels this membrane from the surface of the retina, allowing the retina to “flatten” over the following weeks. Visual recovery is usually very good, occurring progressively over a few weeks to a few months after the surgery.
Macular Hole
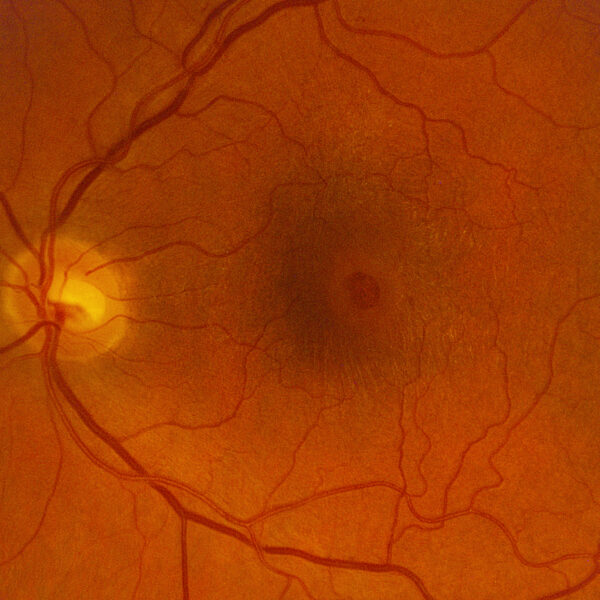 The macula or center part of the retina is responsible for detail vision. In some cases, the vitreous gel that fills the eye can begin to separate from the retina (see PVD) with part of it still adhered to the macula. This causes traction on the macula, and can cause visual distortion or blurring; the condition is referred to as vitreo-macular traction syndrome. As the vitreous finally pulls away from the retina, it can pull a small piece of the retinal tissue away from the macula, leaving a hole.
The macula or center part of the retina is responsible for detail vision. In some cases, the vitreous gel that fills the eye can begin to separate from the retina (see PVD) with part of it still adhered to the macula. This causes traction on the macula, and can cause visual distortion or blurring; the condition is referred to as vitreo-macular traction syndrome. As the vitreous finally pulls away from the retina, it can pull a small piece of the retinal tissue away from the macula, leaving a hole.
Patients with a macular hole report a dark or blurred area in the center vision, usually right at the point of fixation. Symptoms can be similar to macular degeneration, in that faces and text can be missing or blurred, while the outer or peripheral vision is unaffected.
Repair of macular hole consists of vitrectomy or removal of the vitreous gel, and a gas-fluid exchange in which a special type of gas bubble is injected into the eye. During recovery, the patient must maintain a face-down position in order to cause the gas bubble to float upward and hold pressure against the macular hole. This face-down positioning is not easy to endure, but is very important during recovery. Some patients opt to use special positioning equipment to make them more comfortable while recovering. The gas bubble is absorbed slowly over ten to fourteen days, at which point positioning is no longer necessary.
